The persistent worry about having a serious illness and the overwhelming urge to check your symptoms online may signal the complex interplay between OCD and health anxiety—two distinct but often overlapping mental health disorders. Understanding these conditions is crucial for accurate diagnosis and effective treatment, especially when symptoms begin to interfere with daily life.
Introduction to Illness Anxiety Disorder
Mental health disorders, such as obsessive compulsive disorder (OCD) and illness anxiety disorder, can significantly impact daily life and well-being. These conditions can affect everything from personal relationships to work performance, often creating significant distress for those experiencing them.
Health anxiety and OCD are two distinct mental health conditions that involve excessive worry and fear related to health, though they manifest in different ways and have different underlying mechanisms. While both conditions can involve preoccupation with health concerns, understanding the differences between these disorders is crucial for effective diagnosis and treatment.
The Diagnostic and Statistical Manual (DSM) provides healthcare professionals with standardized criteria for diagnosing these conditions. In fact, the most recent edition (DSM-5) reclassified what was previously known as hypochondriasis into two distinct disorders: illness anxiety disorder and somatic symptom disorder.
Seeking help from healthcare providers is essential for managing symptoms and improving quality of life. Without proper treatment, these conditions can become increasingly debilitating, affecting every aspect of a person’s life.
Health Anxiety
Health anxiety involves excessive and persistent worry about having or developing a serious medical condition, often despite medical reassurance that no serious illness exists. This condition goes beyond normal concerns about health and becomes problematic when it significantly interferes with daily functioning.
People with health anxiety often find themselves constantly worrying about illness, disease, and death. This worry can become all-consuming, creating what some describe as “a unique form of torture” that significantly diminishes quality of life. Many individuals with health anxiety believe that intense suffering is inevitable if an illness is identified, and they often view health as a binary state—either you’re 100% healthy or facing imminent death.
Health anxiety typically manifests through several behaviors:
- Excessive medical consultations and repeated visits to the doctor’s office
- Frequent medical tests and examinations
- Constant body checking for signs of illness
- Excessive internet searches about symptoms and diseases
- Seeking reassurance from family members about health concerns
- Avoiding physical activities or situations perceived as health risks
The impact of health anxiety can be profound, leading to social isolation, difficulties maintaining employment, and comorbid conditions such as depression or generalized anxiety disorder. However, effective treatments exist that can help those suffering from health anxiety regain control of their lives.
Illness Anxiety Disorder
Illness anxiety disorder is a specific mental health disorder recognized in the DSM-5, characterized by preoccupation with having or acquiring a serious illness, despite minimal or absent physical symptoms. This preoccupation persists despite appropriate medical evaluation and reassurance.
The diagnostic criteria for illness anxiety disorder include:
- Preoccupation with having or acquiring a serious illness
- Absence of somatic symptoms or, if present, only mild symptoms
- High level of anxiety about health
- Excessive health-related behaviors or maladaptive avoidance
- Illness preoccupation that has persist
- ed for at least six months
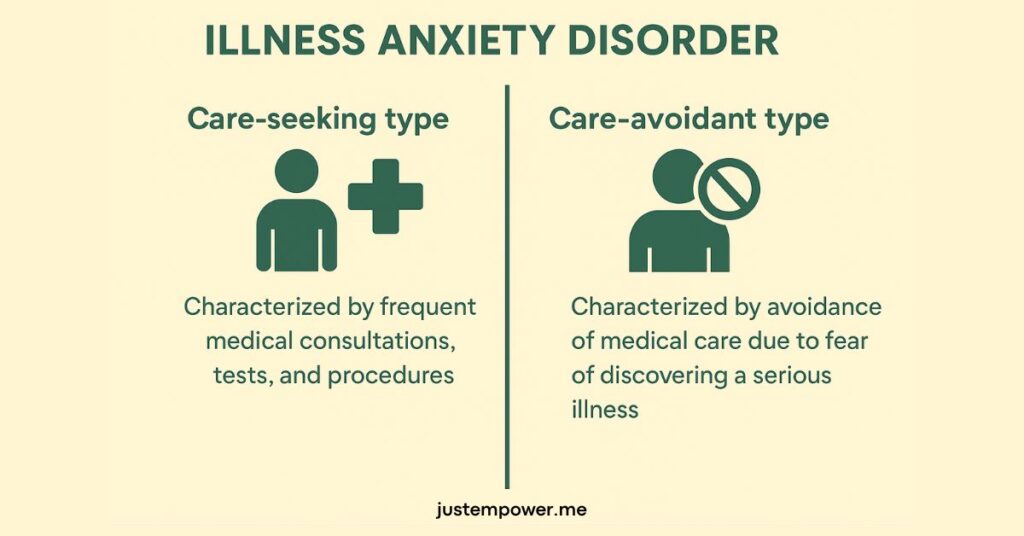
Illness anxiety disorder can present in two distinct ways:
- Care-seeking type: Characterized by frequent medical consultations, tests, and procedures
- Care-avoidant type: Characterized by avoidance of medical care due to fear of discovering a serious illness
People with illness anxiety disorder often experience significant distress and impairment in daily life. They may struggle to maintain relationships as their health concerns dominate conversations, or they might avoid social situations altogether due to fears about their health. The constant worry can lead to problems at work or school, further diminishing quality of life.
Treatment for illness anxiety disorder typically involves a combination of therapy and medication. Cognitive-behavioral therapy can help address catastrophic misinterpretations of bodily sensations, while selective serotonin reuptake inhibitors (SSRIs) may be beneficial in cases with significant comorbid anxiety or depression.
Somatic Symptom Disorder
Unlike illness anxiety disorder, somatic symptom disorder involves real physical symptoms that cause significant distress, though the response to these symptoms is excessive or disproportionate. This condition is characterized by one or more somatic (physical) symptoms that are distressing or result in significant disruption of daily life.
The key feature of somatic symptom disorder is not the symptoms themselves but the way the person responds to them—with disproportionate and persistent thoughts about the seriousness of their symptoms, persistently high anxiety about health, and excessive time and energy devoted to symptoms or health concerns.
Diagnostic criteria for somatic symptom disorder include:
- One or more somatic symptoms that are distressing or disruptive to daily life
- Excessive thoughts, feelings, or behaviors related to these symptoms
- Symptom state that is persistent (typically more than six months)
For example, a person with somatic symptom disorder might experience chronic pain and become so preoccupied with this symptom that they struggle to think about anything else. They might visit multiple doctors seeking a diagnosis, become convinced they have a rare illness despite medical reassurance, and significantly alter their lifestyle due to fear of exacerbating their pain.
Treatment approaches for somatic symptom disorder include cognitive-behavioral therapy focused on changing beliefs about physical symptoms, regular appointments with one primary care provider to reduce doctor-shopping behavior, and mindfulness-based therapies to reduce catastrophic thinking about bodily sensations.
Health Concern OCD
Health concern OCD, also known as health anxiety OCD, is a specific subtype of obsessive compulsive disorder characterized by intrusive, unwanted thoughts about health and illness, followed by compulsive behaviors designed to reduce the associated anxiety. This subtype differs from general health anxiety in important ways.
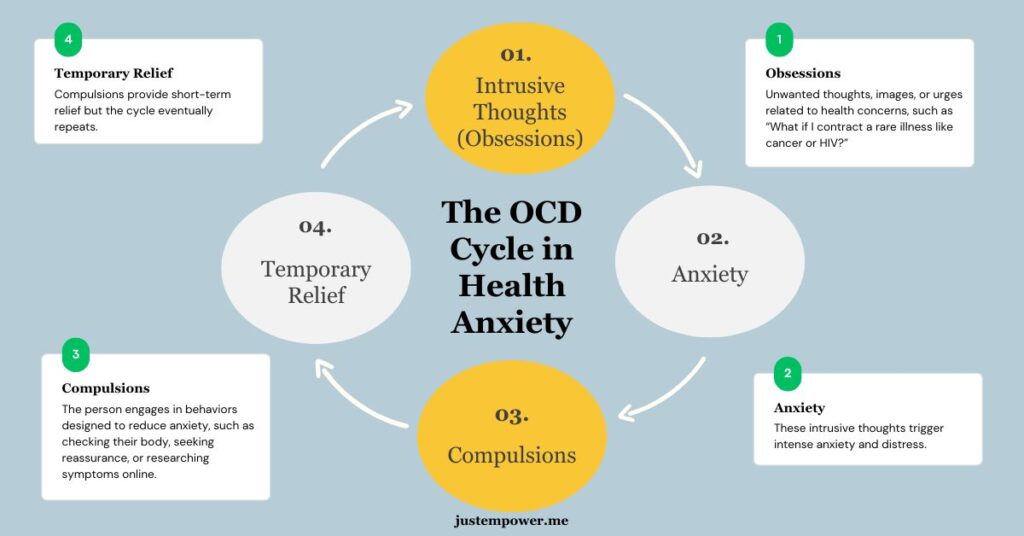
The OCD cycle in health concern OCD typically involves:
- Intrusive thoughts (obsessions): Unwanted thoughts, images, or urges related to health concerns, such as “What if I have cancer?” or “What if I contract a rare illness?”
- Anxiety: These intrusive thoughts trigger intense anxiety and distress
- Compulsions: The person engages in behaviors designed to reduce anxiety, such as checking their body, seeking reassurance, or researching symptoms online
- Temporary relief: Compulsions provide short-term relief, but the cycle eventually repeats
Unlike general health anxiety, where the concern about health stems from a sincere place of worry, in health concern OCD, the thoughts about illness are experienced as intrusive and unwelcome. People with health concern OCD often recognize that their fears are excessive or irrational, but feel unable to control their thoughts or resist their compulsions.
Common obsessions in health concern OCD include fear of having a serious undiagnosed illness, fear of contracting a specific disease like cancer or HIV, and intrusive images of oneself suffering from a serious illness or being terminally ill. These obsessive thoughts can become so severe that individuals become completely housebound due to their fears.
Common Compulsions in OCD
Compulsions in OCD serve as temporary anxiety-reduction strategies but ultimately reinforce the cycle of obsessions and anxiety, creating a pattern that’s difficult to break without proper treatment. These repetitive behaviors or mental acts are aimed at preventing or reducing distress or preventing some dreaded event or situation.
In the context of health anxiety OCD, common compulsions include:
Physical checking compulsions:
- Repeatedly examining parts of the body for signs of illness
- Measuring vital signs repeatedly (e.g., pulse, blood pressure, temperature)
- Monitoring bodily sensations excessively
- Checking for symptoms of a heart attack or other serious condition
Reassurance-seeking compulsions:
- Repeatedly consulting medical professionals
- Asking family members about symptoms
- Seeking multiple medical opinions for the same concern
- Repeatedly describing symptoms to others to gauge their reaction
Information-seeking compulsions:
- Excessively researching symptoms and diseases online
- Reading medical books and journals
- Watching medical TV programs about diseases
- Joining health forums or support groups for diseases one fears having
Avoidance compulsions:
- Avoiding hospitals, doctor’s offices, or medical information
- Avoiding people who are ill
- Avoiding physical activities that increase heart rate or cause new symptoms
- Avoiding certain foods or substances feared to cause illness
These compulsions provide temporary relief from anxiety but maintain the OCD cycle by preventing natural habituation to anxiety and reinforcing the belief that the feared outcome is likely or dangerous. Recognizing these patterns is a critical step in treatment, as these compulsions must be gradually reduced to break the OCD cycle.
Response Prevention for OCD and Health Anxiety
Response prevention is a crucial component of the most effective treatment for OCD, known as Exposure and Response Prevention (ERP) therapy. This technique involves systematically preventing the individual from engaging in their typical compulsive behaviors while exposing them to situations that trigger their obsessions and associated anxiety.
In the context of health anxiety OCD, response prevention might include:
- Refraining from checking one’s body for signs of illness
- Not seeking reassurance from medical professionals or family members
- Avoiding excessive research about symptoms and diseases
- Resisting the urge to perform safety behaviors or rituals related to health concerns
The theoretical foundation of response prevention is based on the principles of habituation and extinction. When a person experiences anxiety triggered by an obsession but refrains from performing their compulsion, they eventually learn that:
- Anxiety naturally decreases over time without compulsions
- The feared consequences do not occur
- They can tolerate uncertainty and distress without resorting to compulsive behaviors
For example, a person with health concern OCD might be asked to deliberately notice a bodily sensation (like a slight headache) without checking medical websites, asking others for reassurance, or performing other compulsions. Initially, this will cause anxiety to spike, but over time, the person learns that they can tolerate this uncertainty without needing to perform compulsions.
The effectiveness of response prevention depends on consistency in applying the technique, the patient’s willingness to tolerate temporary increases in anxiety, and gradual progression from easier to more challenging response prevention exercises. When implemented effectively, response prevention leads to significant reduction in OCD symptoms and greater tolerance for uncertainty—a key skill for managing health anxiety in the long term.
Medical Condition and OCD
Having a medical condition can trigger or exacerbate OCD symptoms, particularly in individuals with health anxiety OCD. This creates a complex situation where distinguishing between appropriate medical concern and excessive anxiety becomes challenging.
Medical conditions can influence the development and expression of OCD in several important ways:
- The experience of a serious illness can create a foundation for catastrophic thinking about health
- Medical procedures, treatments, and healthcare environments become associated with anxiety
- Normal bodily sensations related to the medical condition become misinterpreted as signs of new or worsening illness
- The uncertainty inherent in many medical conditions feeds into OCD’s intolerance of uncertainty
Healthcare professionals with OCD, particularly those working in intensive care settings, may be vulnerable to developing health anxiety OCD due to routine exposure to rare illnesses, death, and permanent suffering in their work environment. Their greater awareness of potential medical complications and rare conditions can fuel catastrophic thinking about their own health.
It is entirely possible to have both a legitimate medical condition and health anxiety OCD simultaneously. This creates significant challenges for both patients and healthcare providers:
- Distinguishing between appropriate medical concern and excessive anxiety
- Addressing medical needs without reinforcing OCD symptoms
- Managing the psychological impact of medical uncertainty
- Balancing thorough medical evaluation with avoiding unnecessary testing that reinforces anxiety
For example, a person diagnosed with a chronic illness might develop excessive worry about potential complications, checking their symptoms far more frequently than medically necessary and seeking repeated medical reassurance despite stable test results. In these cases, collaborative care between mental health and medical providers is essential for effective treatment.
Obsessive Compulsive Disorder OCD Treatment
Effective treatments for obsessive compulsive disorder, including health anxiety OCD, have advanced significantly, with several evidence-based approaches showing substantial success in reducing symptoms and improving quality of life.
Exposure and Response Prevention (ERP) Therapy: ERP remains the gold standard psychological treatment for OCD, with substantial empirical support. This approach involves:
- Systematic exposure to feared situations, thoughts, or sensations without performing compulsions
- Gradual progression through a hierarchy of increasingly challenging exposures
- Learning to tolerate anxiety and uncertainty without resorting to compulsive behaviors
For health anxiety OCD specifically, ERP might include exposure to health-related information without checking or seeking reassurance, deliberately paying attention to bodily sensations without performing checking rituals, and tolerating uncertainty about health status without seeking excessive medical opinions.
Medication: Pharmacological interventions, particularly selective serotonin reuptake inhibitors (SSRIs), play an important role in OCD treatment:
- SSRIs including fluoxetine, fluvoxamine, sertraline, paroxetine, and escitalopram have demonstrated efficacy
- Higher doses than those used for depression are often required for OCD
- Response typically takes 8-12 weeks, with continued improvement over 6 months
- Medication is often combined with ERP for optimal outcomes
Cognitive Therapy: Often combined with ERP, cognitive therapy addresses the dysfunctional beliefs underlying OCD:
- Identifying and challenging catastrophic misinterpretations of bodily sensations
- Addressing perfectionist beliefs about health and illness prevention
- Modifying beliefs about responsibility for preventing illness
- Developing more realistic assessments of health risks and tolerance for uncertainty
Treatment Considerations for Health Anxiety OCD: Specific considerations for treating health anxiety OCD include:
- Clear differentiation from legitimate medical concerns
- Careful coordination with medical providers
- Education about normal bodily sensations and functions
- Addressing fear of death or serious illness that often underlies symptoms
- Developing appropriate health behaviors that avoid both neglect and excessive vigilance
With appropriate treatment, most individuals with OCD, including health anxiety OCD, can expect significant symptom reduction. Treatment outcomes indicate that approximately 70% of patients who complete ERP treatment show clinically significant improvement (Source). Many individuals require ongoing maintenance treatment to sustain improvements over time, but the prognosis for these conditions is generally positive with proper intervention.
What to Do About Illness Anxiety Disorder
OCD and health anxiety represent significant challenges, but with proper diagnosis and treatment, individuals experiencing these conditions can learn to manage symptoms effectively and reclaim their quality of life. Understanding the distinctions between these related but different disorders is essential for accurate diagnosis and appropriate treatment planning.
The evidence clearly supports Exposure and Response Prevention (ERP) therapy as the first-line psychological treatment for OCD, including health anxiety OCD. This approach, often supplemented with medication for moderate to severe cases, has demonstrated robust effectiveness across numerous clinical studies. Cognitive-behavioral approaches that address catastrophic misinterpretations of bodily sensations have shown promising results.
Recovery typically involves not the complete absence of intrusive thoughts or health concerns, but rather a changed relationship with these experiences that allows for greater psychological flexibility and improved quality of life. With comprehensive treatment and ongoing support, individuals can develop greater tolerance for uncertainty and reconnect with valued life activities.
If you recognize symptoms of health anxiety or OCD in yourself or a loved one, seeking help from healthcare providers is an essential first step. A mental health professional who specializes in anxiety disorders can provide an accurate diagnosis and develop an effective treatment plan tailored to your specific situation. Remember that these conditions are treatable, and seeking help is a sign of strength, not weakness.